Endometriosis is a complex and multifactorial disease that affects 1 in 10 Australian women. It occurs when tissue similar to that found in the uterus grows in other areas of the body, often involving multiple organs such as the bowel, bladder, ovaries, appendix and, in some cases, the lungs or diaphragm.
The exact cause is unknown but current research supports the view that endometriosis is an inflammatory condition with potential immune system dysregulation. It was previously viewed solely as a hormonal disease and the only treatment that was often prescribed was surgery and hormonal therapy.
There is still such a lack of awareness, knowledge, funding, research and support around endometriosis.
There are also many misconceptions about this disease:
- Endometriosis affects the whole body, it is not just a reproductive disease.
- The average diagnosis time is 8-10 years from the onset of symptoms and there is currently no cure.
- Endometriosis can only be diagnosed via laparoscopic surgery and is often dismissed for years as just painful periods, misdiagnosed or left undiagnosed.
- Endometriosis is listed as one of the top 20 most painful medical conditions
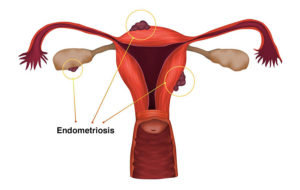
Endometriosis. A condition in which the endometrium, the layer of tissue that normally covers the inside of the uterus, grows outside of it.
Common symptoms include:
- Abdominal pain
- Low back & pelvic pain
- Nerve pain
- Leg & hip pain
- Severe bloating
- Nausea & vomiting
- Brain fog
- Depression and anxiety
- Chronic fatigue
- Memory problems
- Insomnia
- Headaches & migraines
- Dizziness & fainting
- Painful & heavy periods
- Immune system dysfunction
- Chronic pain
- Fibromyalgia
- Vulvodynia
- Pain with sexual intercourse
- Pain with bowel movements & urination
- Diarrhoea & constipation
- IBS & other digestive complaints (reflux, heartburn, loss of appetite)
- Food intolerances
- Infertility
Women with endometriosis often experience severe pain and many of the above symptoms on a daily basis – not just while menstruating. There is no cure for endometriosis yet but having a diagnosis can help in symptom management.
How can Osteopathy help?
With a complex condition like endometriosis, it is vital to take a holistic and multifactorial approach to this disease. It is important to find yourself a team of supportive and skilled medical practitioners that are going to support your individual needs.
As Osteopaths we consider the whole body – how all of the systems interrelate and function together. When treating a woman with endometriosis, we will consider how the musculoskeletal, reproductive, gastrointestinal, respiratory and nervous systems all interact as a holistic unit.
Endometrial lesions often cause adhesions and scar tissue within the pelvic and abdominal cavity, and in some cases the thoracic cage. These adhesions influence how the organs, fascia, nerves, connective tissue and joints are able to move and function.
Osteopathy has been shown to reduce chronic pelvic pain by decreasing pelvic floor tension, improving breathing mechanics, influencing the ligaments that support your organs and improving the mobility of the hips, low back, pelvis and rib cage. Improved function of the musculoskeletal system and nervous system improves pain levels, increases blood flow, decreases inflammation and aids in tissue healing. Osteopaths can also prescribe self-management strategies, home strength and mobility exercises, breathing techniques, tools to support sleep, stress management and ergonomic advice.
It is important to find a GP who has an interest in women’s health or chronic pain and a good gynaecologist who specialises in endometriosis and has experience with excision surgery. Consider addressing lifestyle factors like diet, exercise, sleep patterns and stress management. An osteopath, pelvic floor physiotherapist, acupuncturist, psychologist and naturopath/nutritionist are great additions to your support team.
I will write another post soon about some great management techniques so keep an eye out 👀
The article was written by Emma Berry (Osteopath)

